Introduction
Candida auris is an emerging yeast, responsible for invasive nosocomial infections. This species was first described from an external ear canal drainage sample from a Japanese patient in 2009 [1]. It is currently a global health problem due to its increasing detection across the world, especially with outbreaks of invasive infections in healthcare facilities worldwide. The first hospital outbreaks were reported in 2016 in hospitals in New York, London, and Valencia in Spain. Since then, C. auris has been reported from dozens of countries over six continents [2]. The main monitoring programs are European and American. In the United States, 1 272 cases were identified by the Centers for Disease Control and Prevention CDCs between 2016 and 2020 [2]. In Europe, the European Centre for Disease Prevention and Control ECDC identified 620 cases between 2013 and 2017 [3]. The emergence of C. auris is also alarming because of its potential to present or develop multidrug resistance to antifungals. In addition, it is sometimes difficult to correctly identify C. auris with standard laboratory methods. The overall crude in-hospital mortality rate for C. auris candidemia ranges from 30% to 72% [4,5,6]. C. auris can colonize patients and persist for long periods of time on surfaces, promoting its spread between patients in hospitals [2]. The risk factors for C. auris infection appear to be similar to those of other species of the genus Candida. Several risk factors such as immunosuppression, comorbidities, the presence of indwelling devices (catheters), recent surgery, exposure to broad spectrum antimicrobials, diabetes, parenteral nutrition, cancer and admission to intensive care units or in a specialized care residence, have been reported [7]. C. auris is a global public health issue due to the difficulties in eradicating it once it is present in the hospital environment. Here, we review recommendations for the detection and management of C. auris infections, and measures to implement C. auris outbreak control practices.
Identification
The prevalence of C. auris infections is probably underestimated due to misidentification of this yeast at the species level. Indeed, erroneous identification of C. auris as C. famata, C. haemulonii, C. duoboshaemulonii by commercial microbiological techniques has been reported [8,9,10,11]. Although Matrix-Assisted Laser Desorption/Ionization Time-Of-Flight (MALDI-TOF) is a reliable technique for identification, several studies have demonstrated the existence of erroneous identification of C. auris isolates with MALDI-TOF because C. auris was not registered in the database [7,8,9,10,11,12] . It is therefore essential to verify the presence of C. auris reference spectra in the MALDI-TOF database and to ensure the correct identification of C. auris by testing reference strains [13]. The identification of C. auris by molecular biology is the gold standard. It is generally performed by sequencing of the D1-D2 region of ribosomal DNA 28S. This molecular technique overcomes the weaknesses of existing phenotypic tests to identify C. auris. In addition, it is easy to perform, fast and overcome identification errors [10,14].
Susceptibility to antifungals and treatment
Mortality is very high with rates ranging from 30 to 72%. C. auris has the potential to present or develop multidrug resistance to antifungals. Only 4 classes of drugs are available for the treatment of systemic Candida infections including the azoles (fluconazole, itraconazole voriconazole, posaconazole and isavuconazole), polyenes (amphotericin B), echinocandins (caspofungin, micafungin and anidulafungin) and finally the pyrimidine analogues (flucytosine) [15,16]. A review of the literature allowed us to take stock of antifungal resistance by observing the distribution of minimal inhibition concentration (MIC) according to geographical origin [17,18,19,20,21,22,23]. For fluconazole, all strains have high MIC regardless of geographical origin. In the United States, 96% of strains were resistant to fluconazole with MIC>64 µg/mL [21,22]. For other azoles, especially voriconazole, MIC were lower (no more than >16 µg/mL). A meta-analysis showed that one third of the strains were resistant to voriconazole in the word (38% of 742 cases) [24]. This proportion appears to be higher in Western countries (United States, United Kingdom) [19,20,21,22]. Amphotericin B resistance is the third in terms of frequency (26% of 742 C. auris strains all over the world). The proportion of resistant strains is particularly high in the United States with MIC ranging from 1 µg/mL to 8 µg/mL [20,21,22]. Flucytosine has not yet been widely assessed but resistance has been reported in India with MIC of up to 64 µg/mL [23]. Finally, for echinocandins, strains are generally susceptible but resistance begins to emerge, especially in India with some strains exhibiting MIC of 8 to 16 µg/mL [23]. India is the geographical location with significant resistance rates for all four classes of antifungals. These resistances are most often associated within two classes in 23% of cases, three classes in 2% of cases and all classes in 0,3% [23]. By now there is no MIC breakpoints to define the susceptibility of C. auris to antifungals. The breakpoints used are those found in the literature and suggested by the CDC : fluconazole ≥32 µg/mL, amphotericin B≥2 µg/mL, caspofungin ≥2 µg/mL, micafungin ≥4 µg/mL and anidulafungin ≥4 µg/mL [16,25]. Currently, there are recommendations from the CDCs regarding the treatment of C. auris infection. The first line treatment is an echinocandin [26]. Amphotericin B may be an alternative for patients unresponsive to treatment with echinocandins, depending on the MIC [13,27]. It has been shown that resistance can evolve very quickly in this species. It is therefore recommended to continuously monitor the evolution of resistance in patients colonized or infected with C. auris [28].
Virulence and sources of infection
Some species of the genus Candida are present in the commensal state in most human beings thanks to the great adaptability of their survival capacities in the human body [29]. The most common species responsible for invasive infections are C. albicans, C. tropicalis, C. parapsilosis and C. glabrata [29]. For these species, patients become infected with their own strains, as opposed for C. auris where patient-to-patient transmission is possible [30]. Several studies have been carried out to characterize the virulence factors of C. auris [30] and showed that C. auris can produce phospholipases and proteases, although in a strain-dependent manner. C. auris is also able to form biofilms and adhere to material, especially catheters, but this capacity is less strong compared to that of C. albicans [31,32,33].
Studies performed in India, Pakistan, Venezuela and Colombia have reported outbreaks of C. auris infection or colonization. Infections were observed several days to a few weeks after hospitalization in predisposed patients [34]. This suggests an exogenous source of contamination associated with poor practice of recommendations for combating healthcare-related infections. Another study carried out in 4 hospitals from Colombia showed the detection of C. auris both on bed rails, medical equipment and doorknobs, and isolated the yeast on the hands and groin of healthcare professionals. These results suggest that colonized patients can spread C. auris in their immediate environment and contaminate surfaces at varying distances resulting in a risk of continued transmission [35,36]. Environmental factors play a role in hospital outbreaks. This results in prolonged survival of C. auris in hospital settings, due to skin colonization of patients and asymptomatic carriers [32]. It is therefore necessary to implement strict control measures to prevent the transmission of C. auris. The hygienic measures include isolation of patients and their contact, the wearing of personal protective clothing by the nursing staff, the screening of patients and environmental measures such as cleaning the environment with chlorine-based disinfectants and final decontamination with hydrogen peroxide or ultraviolet light. These measures could prevent the transmission of C. auris and would also reduce infections due to many other nosocomial pathogens [37].
Epidemiology
Phylogeographic clades
The CDC explored the molecular epidemiology of C. auris infections by whole genome sequencing (WGS) of 47 isolates collected from Pakistan, India, South Africa and Venezuela from 2012 to 2015 and the type strain from Japan. Phylogenetic analysis identified a strong phylogeographic structure comprising 4 clades of C. auris: South Asia, East Asia, Africa and South America. These clades are separated by tens of thousands of single-nucleotide polymorphisms while the genetic diversity between isolates within a given clade was very low [8,34]. A recent study proposed a potential fifth clade for an isolate from Iran that was found to be genetically distinct from the four known clades with a difference of >200 000 single-nucleotide polymorphisms [38].
Outbreaks
The worldwide epidemiology of C. auris remains poorly understood; in particular the incidence and the prevalence rate are not available due to identification difficulties. In retrospective studies, the first C. auris infections were documented in South Korea in 1996 [39,40]. C. auris is now present over all the 6 continents [41]. Several large outbreaks in healthcare facilities have been reported in Europe [42]. In India, the first outbreak was described in 2013 [43]. In a tertiary care hospital, seven cases of fungemia, three cases of diabetic gangrenous foot, and one case of bronchopneumonia were reported. The main risk factors of the patients were a broad spectrum antibiotic therapy, the existence of an immunosuppression or the presence of a catheter.
The first outbreak of C. auris in America occurred in an intensive care unit at the Maracaibo tertiary hospital in Venezuela between March 2012 and July 2013 [44]. It involved 18 patients, 13 of which were pediatric; most of them received broad-spectrum antibiotics, had intravenous catheters, and were on mechanical ventilation. Isolated cases of infection by C. auris have been reported in various cities of Columbia since 2013: between 2015 and 2016, 27 isolates of C. auris were found in Barranquilla [44]; in Cartagena, 5 cases of disseminated infection during an outbreak in a pediatric intensive care unit were reported in August 2016. The main risk factors found were the use of a central venous catheter, mechanical ventilation, and urinary catheter [44]. In the US, all cases occurred after June 2015. As of July 31 2020, 1 272 confirmed clinical cases of C. auris have been identified. Cases have been reported in 14 states, mainly from New York City, Illinois, and New Jersey [2].
In Europe, there were 3 major outbreaks. The first one occurred in a cardio thoracic center in London between April 2015 and July 2016 with 50 C. auris cases whose 44% (22/50) developed possible or proven C. auris infection [45]. The second outbreak was reported in the university hospital of Valencia, Spain, between April 2016 and March 2017 [46]. Among the 140 patients with C. auris positive cultures, 41 developed candidemia episodes. All the patients had undergone surgery and were treated with anidulafungin and micafungin. Finally, the last outbreak also took place in Oxford. A cluster of C. auris infections was identified in the Neurosciences Intensive Care Unit of the Oxford University Hospitals, United Kingdom [19]. Seventy patients were identified as being colonized or infected with C. auris and invasive C. auris infection developed in 7 patients. C. auris was detected from reusable equipment, including multiple axillary skin-surface temperature probes. In France, only sporadic cases have been reported [47], with two cases between 2013 and 2017 [3] and 1 case between January 2018 and May 2019 [48].
Other hospital outbreaks have occurred around the world [49,50,51,52,53]. The main outbreaks are summarized in Table I.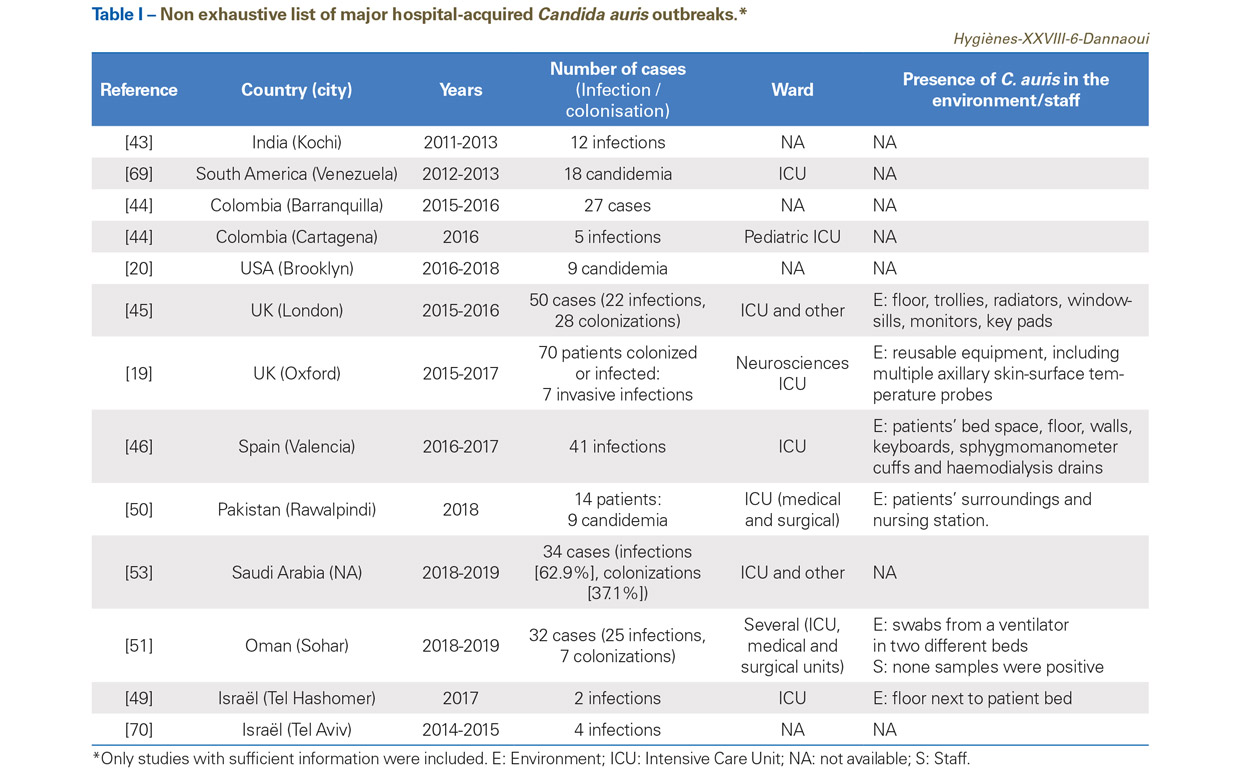
Methods for infection prevention and control
C. auris is responsible for serious infections and outbreaks in hospitals. The difficulty of a proper identification of this species lead to several consequences, first, at an individual level, with the delay in setting up an effective treatment for the patient, second, at a collective level with a delay in the detection of an outbreak and therefore delayed implementation of appropriate control measures [54]. C. auris is able to colonize the skin of healthy carriers but also to contaminate and persist for several weeks in the care environment [54]. The precise mode of transmission is not known [28]. It therefore seems essential to put in place effective measures to prevent and control C. auris infections.
Public Health England (PHE) and the CDCs have recommended strategies similar to the measures put in place for highly antibiotic-resistant bacteria (BHRe). First of all, it is necessary to respect standard hygiene precautions but also additional contact type precautions: isolation of patients and their contact, wearing of personal protective clothing by the nursing staff, individual room only, reinforced hand hygiene.
Case detection and identification
The European (ECDC), English (PHE) and American (CDCs) recommendations concerning screening are almost identical. The measures consist of screening on admission patients who have been transferred from or who have stayed in a hospital where patients are known to be infected or colonized by C. auris [55]. Regarding screening sites, the main recommended ones are the axilla and groin regions [37]. Other sites are possible depending on the clinical context (mouth, external ear canals, urine, wounds, and rectum). The CDCs recommend that screening of colonized patients should be continued for 1 to 3 months [4,6,55].
Hand hygiene
Healthcare personnel in contact with patients infected or colonized with C. auris should follow standard hand hygiene measures, namely cleaning with soap and water or with alcohol-based hand sanitizer. It should be stressed that wearing gloves is not a substitute for hand hygiene [37].
Transmission-based precautions
Patients colonized or infected with C. auris should be managed using contact precautions and with enhanced barrier precautions. Infected or colonized patients should be isolated in a single room if possible. If a limited number of single rooms is available, the single rooms must be prioritized for patients with the higher risk of transmission, namely those with uncontained secretions or excretions or diarrhea [37]. Patient cohorting is also possible. The problem with this measure is that patients are often colonized with different combinations of resistant pathogens. For the choice of rooms, it is therefore possible that contact precautions are considered for a single pathogen (C. auris) without taking into account the measures necessary for the other pathogens [56]. The English guidelines (PHE) specify that the lifting of geographic isolation is possible after 3 negative screening results while 2 negative screening results over one week are sufficient according to the CDC recommendations [55]. Transmission-based precautions should be continued for as long as a patient is colonized with C. auris. However, the average duration of this colonization remains unknown [56].
Environmental cleaning and disinfection
C. auris is able to adhere and persist in the hospital environment, which is why it is important to carry out a rigorous environmental cleaning and disinfection to avoid new hospital outbreaks. The quaternary ammonia compounds, which are the most commonly disinfectants used in healthcare settings, are ineffective against C. auris [57,58,59]. It has also been shown that fungicidal disinfectant and antiseptic compounds used for C. albicans may not be effective against C. auris [59,60]. To act against C. auris, the CDCs recommend the use of an Environmental Protection Agency (EPA)-registered hospital-grade disinfectant known to be effective against Clostridioides difficile spores [37,56]. Among these agents, sodium hypochlorite can be used. To be effective, the compound must be applied for the correct contact time [37]. Furthermore, the EPA developed a standardized quantitative disk carrier method that can be used to evaluate disinfectant efficacy against C. auris [56,61]. Regarding other measures such as vaporized hydrogen peroxide, ultraviolet light, ionization and titanium dioxide/ ultraviolet light, further studies are needed to verify their effectiveness against C. auris [37,62,63].
Decolonization
Regarding the decolonization of patients carrying C. auris, a method used during an outbreak in the United Kingdom, using wipes of 2% chlorhexidine gluconate or aqueous 4% chlorhexidine formulation was effective [56]. However there is yet no clinical study to confirm these results [55]. By now, there is no established protocol for the decolonization of patients with C. auris [56].
Communication and education
It is important to identify patients colonized with C. auris for implementing appropriate infection prevention and control practices. Confirmed cases (infected or colonized) should be reported to National surveillance programs. In USA, the state or local health department should follow the CDCs’ Interim Guidance for a Public Health Response to Contain Novel or Targeted Multidrug-resistant Organisms [37,55]. Appropriate communication and education of HCP should be carried out when a patient is found to be infected or colonized with C. auris [56].
C. auris and the pandemic of Covid-19
End of 2019-beginning of 2020, the emergence of severe acute respiratory syndrome coronavirus 2 (Sars-CoV-2) has caused the Covid-19 pandemic. It is known that mechanically ventilated patients with Covid-19 are at higher risk of colonization and infection by C. auris [64,65]. Covid-19 patients who are pre-colonized with C. auris and with indwelling devices such as catheters have higher risks of C. auris bloodstream and urinary tract infections [66]. A recent study carried out in a Covid-19 Intensive Care Unit in India reported bloodstream infection by C. auris [67]. In this study, candidemia was detected in 2.5% of the 596 patients and C. auris was the predominant agent for 67% of those patients [67]. In a recent report, it was also highlighted that the fecal fungal microbiomes change in Covid-19 patient. Indeed, there is an increased prevalence of opportunistic fungal pathogens such as C. auris, C. albicans, and Aspergillus fumigatus [68]. All these studies showed the Covid-19 pandemic may provide ideal conditions for outbreaks of C. auris in healthcare facilities. It is therefore important to continue close monitoring of C. auris at a time when Sars-CoV-2 is present worldwide.
Conclusion
Candida auris is a yeast now present over all continents. Because of its potential to present or develop multidrug resistance to antifungals and its persistence in healthcare settings, it is important to do everything possible to achieve a timely diagnosis. This requires rapid and reliable identification tools. In addition, the management of healthcare associated infections and outbreaks requires good communication, education of healthcare personnel and the implementation of specific measures to control the spread of this fungus.